Carotid Bruit AND symptoms suggestive of Carotid Stenosis; Degree of stenosis by atherosclerotic Plaque. Minimum stenosis causing bruit: 50% (75% (1.5 mm lumen) Location. Plaque involves posterior wall of common carotid; Affects bifurcation and flow into internal carotid. Carotid Pulse Used during emergency situations and when performing cardiopulmonary resuscitation (CPR), is found between the larynx and sternocleiomastoid muscle in the front side of the neck on either side of the trachea. When measuring the pulse at the carotid site, compress only one side at a time.
Overview
What are the carotid arteries?
Arteries carry oxygen-rich blood away from the heart to the head and body. There are two carotid arteries (one on each side of the neck) that supply blood to the brain. The carotid arteries can be felt on each side of the lower neck, immediately below the angle of the jaw.
The carotid arteries supply blood to the large, front part of the brain, where thinking, speech, personality and sensory and motor functions reside.
The vertebral arteries run through the spine and supply blood to the back part of the brain (the brainstem and cerebellum).
What is carotid artery disease?
Carotid artery disease, also called carotid artery stenosis, is the narrowing of the carotid arteries, usually caused by atherosclerosis. Atherosclerosis is the buildup of cholesterol, fat and other substances traveling through the bloodstream, such as inflammatory cells, cellular waste products, proteins and calcium. These substances stick to the blood vessel walls over time as people age, and combine to form a material called plaque.
Plaque buildup can lead to narrowing or blockage in the carotid artery which, when significant, can put an individual at increased risk for stroke.
Symptoms and Causes
What are the symptoms?
There may not be any symptoms of carotid artery disease. However, there are warning signs of a stroke. A transient ischemic attack (also called TIA or 'mini-stroke') is one of the most important warning signs of a stroke. A TIA occurs when a blood clot briefly blocks an artery that supplies blood to the brain. The following symptoms of a TIA, which are temporary and may last a few minutes or a few hours, can occur alone or in combination:
Where Is The Carotid Pulse Site Quizlet
- Sudden loss of vision or blurred vision in one or both eyes
- Weakness and/or numbness on one side of the face, or in one arm or leg, or one side of the body
- Slurred speech, difficulty talking or understanding what others are saying
- Loss of coordination
- Dizziness or confusion
- Difficulty swallowing
A TIA is a medical emergency, since it is impossible to predict if it will progress into a major stroke. If you or someone you know experiences these symptoms, get emergency help (Call 9-1-1 in most areas). Immediate treatment can save your life or increase your chance of a full recovery.
TIAs are strong predictors of future strokes; a person who has experienced a TIA is 10 times more likely to suffer a major stroke than someone who has not experienced a TIA.
What is a stroke?
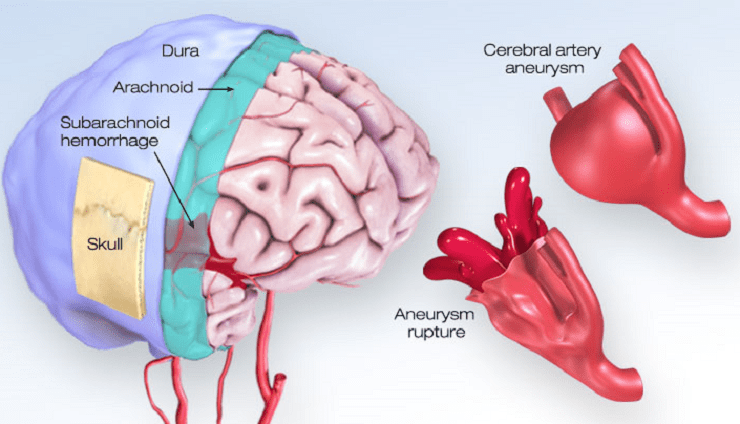
A stroke, or 'brain attack,' occurs when a blood vessel in the brain becomes blocked or bursts. The brain cannot store oxygen, so it relies on a network of blood vessels to provide it with blood that is rich in oxygen. A stroke results in a lack of blood supply, causing surrounding nerve cells to be cut off from their supply of nutrients and oxygen. When tissue is cut off from its supply of oxygen for more than 3 to 4 minutes, it begins to die.
A stroke can occur if:
- The artery becomes extremely narrowed by plaque
- A piece of plaque breaks off and travels to the smaller arteries of the brain
- A blood clot forms and blocks a narrowed artery
A stroke also can occur as a result of other conditions, such as sudden bleeding in the brain (intracerebral hemorrhage), sudden bleeding in the spinal fluid space (subarachnoid hemorrhage), atrial fibrillation, cardiomyopathy, or blockage of the tiny arteries inside the brain.
Diagnosis and Tests
How is carotid artery disease diagnosed?
There may not be any symptoms of carotid artery disease. If you are at risk, it is important to have regular physical exams.
A doctor will listen to the arteries in your neck with a stethoscope. An abnormal rushing sound, called a bruit (pronounced BROO-ee), may indicate carotid artery disease. However, bruits are not always present when there are blockages, and may be heard even when the blockage is minor.
Carotid Pulse Definition
Diagnostic tests include:

- Carotid duplex ultrasound: An imaging procedure that uses high-frequency sound waves to view the carotid arteries to determine if there is narrowing. This is the most common test utilized to evaluate for the presence of carotid artery disease.
- Carotid angiography(carotid angiogram, carotid arteriogram, carotid angio): During this invasive imaging procedure, a catheter (thin, flexible tube) is inserted into a blood vessel in the arm or leg, and guided to the carotid arteries with the aid of a special X-ray machine. Contrast dye is injected through the catheter while X-rays of the carotid arteries are taken. This test may be performed to evaluate or confirm the presence of narrowing or blockage in the carotid arteries, determine the risk for future stroke and evaluate the need for future treatment, such as carotid stenting or surgery.
- Magnetic resonance angiogram (MRA): MRA is a type of magnetic resonance image (MRI) scan that uses a magnetic field and radio waves to provide pictures of the carotid arteries. In many cases, MRA can provide information that cannot be obtained from an X-ray, ultrasound, or computed tomography (CT) scan. This test can provide important information about the carotid and vertebral arteries and the degree of stenosis.
- Computerized tomography (CT Scan): A CT of the brain may be performed if a stroke or TIA is suspected to have already occurred. During a CT scan, X-rays pass through the body and are picked up by detectors in the scanner, which produce three-dimensional (3D) images on a computer screen. Depending on the type of scan you need, a contrast material might be injected intravenously (into a vein) so the radiologist can see the body structures on the CT image. This test may reveal areas of damage in the brain.
- Computed tomography angiogram(CTA): A test that uses advanced CT technology, along with intravenous (IV) contrast material (dye), to obtain high-resolution, 3D pictures of the carotid arteries. CTA images enable physicians to determine the degree of stenosis in the carotid and vertebral arteries and can also assess leading to these arteries as well as the blood vessels in the brain.
Management and Treatment
How is carotid artery disease treated?
Carotid artery disease is treated by:
- Making lifestyle changes
- Taking prescribed medications
- Having procedures as recommended
Lifestyle changes
To prevent carotid artery disease from progressing, these lifestyle changes are recommended by your doctor and the National Stroke Association:
- Quit smoking and using tobacco products.
- Control high blood pressure, cholesterol, diabetes, and heart disease.
- Have regular checkups with your doctor.
- Have your doctor check your lipid profile and get treatment, if necessary to reach a lipid goal of LDL less than 100 and HDL greater than 45 (your doctor may adjust these goals based on additional risk factors and/or medical history).
- Eat foods low in saturated fats, cholesterol, and sodium.
- Achieve and maintain a desirable weight.
- Exercise regularly - at least 30 minutes of exercise most days of the week.
- Limit the amount of alcohol you drink. Excessive alcohol use is defined as drinking more than three drinks per day. (One drink equals 12 ounces of beer or wine cooler, 5 ounces of wine, or 1.5 ounces of 80-proof liquor.)
- Manage other risk factors:
Medications
Anti-platelet medications:All patients with carotid artery disease should take an anti-platelet medication to reduce the risk of stroke and other cardiovascular disease complications. The most commonly used anti-platelet medication is aspirin.
Other drugs that work to keep platelets from 'sticking together' include clopidogrel (Plavix) and dipyridamole (Persantine), which may be prescribed alone or in combination with aspirin to reduce your risk of stroke. In some cases, the anticoagulant medication warfarin (Coumadin) may be prescribed to thin your blood and reduce the risk of blood clots.
Tissue plasminogen activator (t-PA): A clot-dissolving medication approved by the U.S. Food and Drug Administration (FDA) for the treatment of strokes caused by blood clots (ischemic strokes). Eighty percent of all strokes are ischemic. T-PA only works if it is given within three hours of the start of stroke symptoms.
Treatment procedures
Carotid Stenting
If there is severe narrowing or blockage in the carotid artery, a procedure may be necessary to open the artery and increase blood flow to the brain, to prevent a future stroke.
If you have symptoms related to carotid artery narrowing, you will likely need to have either carotid endarterectomy or carotid stenting to correct the narrowing in the artery and reduce your risk of stroke. Your vascular specialist will evaluate you to recommend the best treatment for your situation.
If you have carotid narrowing without symptoms, your vascular specialist will evaluate your test results and risk status to make a recommendation as to whether medical therapy, carotid stenting or carotid endarterectomy would be the best option.
Carotid endarterectomy is the traditional surgical treatment for carotid artery disease. Carotid endarterectomy has been proven to be beneficial for symptomatic patients with a 50 percent or greater carotid stenosis (blockage) and for asymptomatic patients with a 60 percent or greater carotid stenosis.
Carotid endarterectomy can be performed under general anesthesia (the patient is asleep) or local anesthesia with intravenous sedation. During the procedure, an incision is made in the neck at the site of the carotid artery blockage. The surgeon removes the plaque from the artery and when the plaque removal is complete, the surgeon stitches the vessel closed. Blood flow to the brain is restored through its normal path.
Carotid angioplasty and stenting has been FDA-approved as a treatment option for some patients with carotid artery disease. Please talk to your doctor to determine if you are eligible.
The carotid angioplasty and stenting procedure is performed while the patient is awake, but sedated. During the procedure, a balloon catheter is inserted through a sheath in a blood vessel. With X-ray guidance, the catheter is placed through the blood vessel and directed to the carotid artery at the site of the blockage or narrowing. A specially designed guidewire with a filter is placed beyond the area of blockage or narrowing.
Once in place, the balloon tip is inflated for a few seconds to open or widen the artery. The filter (called the embolic protection device) collects any debris that may break off of the blockage. A stent (a small mesh tube) is placed in the artery and opens to fit the size of the artery. The stent stays in place permanently and acts as a scaffold to support the artery walls and keep the artery open. After several weeks, the artery heals around the stent.
Research has shown that carotid stenting, when used with the embolic protection device, was as safe and effective as carotid endarterectomy in high-risk surgical patients.Recovery from both the carotid endarterectomy and carotid angioplasty and stenting procedures generally requires a one-night hospital stay. Patients often return to regular activities within one to two weeks after these procedures.
Follow-up care
Your doctor will want to see you on a regular basis for a physical exam and possibly to perform diagnostic tests. Your doctor will use the information gained from these visits to monitor the progress of your treatment. Check with your doctor to find out when to schedule your next appointment.
Prevention
What are the risk factors for carotid artery disease?
The risk factors that have been linked to the development of atherosclerosis include:
- Family history of atherosclerosis (either carotid artery disease or coronary artery disease or elsewhere in the vascular system)
- Age: In general, the risk of atherosclerosis increases as we age, and in particular, men under age 75 have a greater risk of developing carotid artery disease than women, but after age 75, women have a greater risk than men
- High levels of low density lipoprotein (LDL, bad cholesterol) and triglycerides in the blood. However, this link is not as strong as it is for coronary artery disease
- Sedentary lifestyle
Typically, the carotid arteries become diseased a few years later than the coronary arteries. People who have coronary artery disease, and atherosclerosis elsewhere (such as peripheral artery disease or PAD) have a higher risk of developing carotid artery disease.
Resources
Doctors vary in quality due to differences in training and experience; hospitals differ in the number of services available. The more complex your medical problem, the greater these differences in quality become and the more they matter.
Clearly, the doctor and hospital that you choose for complex, specialized medical care will have a direct impact on how well you do. To help you make this choice, please review our Miller Family Heart, Vascular & Thoracic Institute Outcomes.
Cleveland Clinic Heart, Vascular & Thoracic Institute Vascular Medicine Specialists and Surgeons
Choosing a doctor to treat your vascular disease depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with all types of vascular disease, including blood clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular disease. In addition, the Non-Invasive Laboratory includes state-of-the art computerized imaging equipment to assist in diagnosing vascular disease, without added discomfort to the patient. Call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an appointment online.
Department of Vascular Surgery: surgery evaluation for surgical treatment of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, toll-free 800-223-2273, extension 44508 or request an appointment online.
You may also use our MyConsult second opinion consultation using the Internet. The Heart, Vascular & Thoracic Institute also has specialized centers and clinics to treat certain populations of patients:

Learn more about experts who specialize in the diagnosis and treatment of vascular and arterial disease.
See About Us to learn more about the Sydell and Arnold Miller Heart, Vascular & Thoracic Institute.
Contact
If you need more information, click here to contact us, chat online with a nurse or call the Miller Family Heart, Vascular & Thoracic Institute Resource & Information Nurse at 216.445.9288 or toll-free at 866.289.6911. We would be happy to help you.
Becoming a Patient
Treatment Options
Additional information about vascular treatment options can be found at:
Treatment Guides
Diagnostic Tests
Diagnostic tests are used to diagnose your abnormal heartbeat and the most effective treatment method.
Webchats
Our webchats and video chats give patients and visitors another opportunity to ask questions and interact with our physicians.
- Vascular Disease, Peripheral Arterial Disease & Thrombosis webchats and video chats
Videos
Interactive Tools
Resource Links
- Visit Health Essentials - Read articles on vascular disorders and healthy living on Health Essentials
- American Stroke Association *
- American Heart Association *
- Vascular Cures*
- VascularWeb - Resources for Vascular Disease and Treatment*

*A new browser window will open with this link.
The inclusion of links to other websites does not imply any endorsement of the material on those websites nor any association with their operators.
Surgical Outcomes
Why choose Cleveland Clinic for your care?
Radial Apical Carotid Pulse Sites
Our outcomes speak for themselves. Please review our facts and figures and if you have any questions don't hesitate to ask.
Key Difference – Carotid Artery Pulsation vs Jugular Vein Pulsation
Pulse in general terms can be defined as the transfer of pressure waves inside blood vessels. Carotid pulse is when these pressure waves are moving across the carotid artery. Similarly when the pressure waves move through the internal jugular vein that is known as the jugular venous pulse (JVP). Carotid pulse is an arterial pulse whereas JVP is a venous pulse. This is the key difference between carotid pulse and JVP.
CONTENTS
1. Overview and Key Difference
2. What is Carotid Artery Pulsation
3. What is Jugular Vein Pulsation
4. Side by Side Comparison – Carotid Artery Pulsation vs Jugular Vein Pulsation in Tabular Form
5. Summary
What is Carotid Artery Pulsation?
The carotid artery is one of the major arteries which branches off from the aorta. Assessment of carotid pulse is a part of the routine examination. But some of the clinicians oppose the assessment of carotid pulse based on the possibility of having complications such as transient ischemic attacks, induce reflex and vagally mediated bradycardia. Carotid pulse is the pulse of choice in examining a patient who has had a cardiac arrest.
Surface marking,
- At the angle of the jaw anterior to the sternocleidomastoid muscle.
Examination sequence,
- Carotid pulse on both sides should never be assessed simultaneously.
- The procedure should be explained to the patient.
- Ask the patient to lie in a semirecumbent position.
- Place the tip of the fingers between larynx and the anterior border of sternocleidomastoid and fell the pulse.
- Listen for bruits over the carotid pulse using the stethoscope.
What is Jugular Vein Pulsation?
The pressure inside the jugular vein can be approximated by the assessment of jugular vein pulsation (JVP). The normal waveform produces two peaks per minute. JVP reflects the right atrial pressure. The sternal angle is about 5 cm above the right atrium. Therefore, when the patient lies at an angle of 45 to the horizontal JVP should be checked roughly 4cm above the sternal angle. When the JVP is low patient has to lie flat for it to be seen, and when the JVP is high patient should sit upright.
Examination sequence,
- JVP is best observed on the right side
- Position the patient supine, reclined at 45 and place a pillow underneath to relax the sternocleidomastoid muscles.
- Observe the patient’s neck and identify JVP either in the suprasternal notch or behind the sternocleidomastoid.
- Vertical height between the upper end of the pulse and sternal angle is taken as the JVP
A normal JVP wave has 2 peaks per cardiac cycle. The ‘a’ wave corresponds to the atrial constriction and occurs just before the first heart sound. The other peak which is known as the ‘v’ wave occurs during the ventricular systole when the ventricular filling happens.
What is the Difference Between Carotid Artery Pulsation and Jugular Vein Pulsation?
Carotid Artery Pulsation vs Jugular Vein Pulsation | |
| Carotid pulsation is an arterial pulse. | Jugular vein pulsation is a venous pulse. |
| Number of Peaks | |
| There is only one peak per cardiac cycle. | There are two peaks per cardiac cycle. |
| Palpability | |
| Carotid pulse is palpable. | JVP is impalpable. |
| Impact of the Pressure | |
| Pulsation is not affected by the pressure at the root of the neck. | Pulse is reduced by an increase in the pressure at the root of the neck. |
| Respiration | |
| Carotid pulse does not depend on respiration. | JVP varies with respiration. |
| Impact of Position | |
| Pulse does not change the position of the patient | Pulse changes with the position of the patient. |
| Abdominal Pressure | |
| Pulse is independent of the abdominal pressure. | Pulse increases with an increase in the abdominal pressure. |
Summary – Carotid Artery Pulsation vs Jugular Vein Pulsation
The transfer of pressure waves across carotid artery and the internal jugular vein is respectively known as the carotid pulse and JVP. Carotid pulse is an arterial pulse whereas JVP is a venous pulse. This is the major difference between these two terms.
Download the PDF Version of Carotid Artery Pulsation vs Jugular Vein Pulsation
You can download PDF version of this article and use it for offline purposes as per citation note. Please download PDF version here Difference Between Carotid Artery Pulsation and Jugular Vein Pulsation
Reference:
1.Douglas, Graham, et al., editors. Macleod’s Clinical Examination. 2013.
Image Courtesy:
1.’Carotidian pulse’By Rama, (CC BY-SA 3.0) via Commons Wikimedia
2.’Jugular Venous Pulse’ By Ecgtocardiology – Own work, (CC BY-SA 3.0) via Commons Wikimedia
Related posts:
